I slept last night.
Not the fitful, sweaty, heart-pounding kind of sleep I've gotten used to. Real sleep. The kind where you close your eyes and then it's morning and you feel like a person instead of a haunted house.
I kept food down yesterday. And the day before that. After weeks of daily vomiting, I ate meals and they stayed where meals are supposed to stay.
No doctor did this for me. I did this for me.
The Breakthrough
For years, I've collected diagnoses like the world's worst trading cards. POTS. Gastroparesis. Interstitial cystitis. Fibromyalgia. IBS. Migraines. MCAS. Pelvic congestion syndrome. Anxiety. Depression. The list goes on. Dozens of specialists, each one seeing their piece of the puzzle, none of them seeing the whole picture.
This week, I finally saw the whole picture. And I saw it because I refused to stop looking.
All of my conditions trace back to one thing: my connective tissue is built differently. The collagen that holds my body together (my blood vessels, my gut, my bladder, the sheaths around my nerves) is too stretchy, too fragile. This is hypermobile Ehlers-Danlos Syndrome, or hEDS. It's genetic. It affects everything.
When your blood vessels are too stretchy, blood pools in your legs instead of returning to your heart. Your heart races trying to compensate. That's my POTS. When your gut is structurally different and the nerves controlling it are embedded in faulty tissue, food doesn't move through properly. That's my gastroparesis. When your bladder wall is fragile and the immune cells living in it are constantly overreacting, you get urgency, frequency, and pain. That's my interstitial cystitis.
The immune cells overreacting? Those are mast cells. They live in connective tissue. When that tissue is abnormal, they get irritated and release chemicals they shouldn't like histamine, inflammatory molecules, things that make your heart race and your gut seize up and your brain feel like it's wrapped in cotton. That's Mast Cell Activation Syndrome, or MCAS.
One underlying condition. Not sixty billion separate diseases. One body, doing exactly what a body with faulty connective tissue would do.
What the Doctors Missed
Six months ago, I was prescribed Duloxetine, an SNRI antidepressant. My providers meant well. SNRIs are often used for chronic pain and for depression.
But here's what nobody checked: SNRIs are contraindicated in hyperadrenergic POTS. The kind of POTS I have. The Vanderbilt Autonomic Dysfunction Center (one of the leading research institutions for dysautonomia) explicitly warns against them because they increase norepinephrine, which is already sky-high in people like me.
Six months after starting Duloxetine, my gastroparesis, which had been in remission for three years after surgery, came roaring back. I started vomiting daily. I lost 14 pounds. I developed new nerve pain. I couldn't keep pills down to treat any of it.
I brought this research to my provider. Cited my sources. Explained the timeline. Asked for help tapering off the medication safely.
"I'm not going to take your recommendations."
That's what he said. He called standard lab tests "Mayo Clinic level." He offered to see me in clinic when I'd already told him I was too dizzy to drive.
So I Did It Myself
When you can't keep pills down, you have to get creative. When your doctors won't help you taper off a medication that's making you sicker, you have to figure it out yourself.
I researched safe tapering methods for Duloxetine. The medication comes in capsules filled with tiny beads... it's designed this way because it's extended-release. The standard doses are too far apart for gradual tapering, which is why so many people struggle with SNRI withdrawal. The medical system's solution is usually "just push through it" or "that's not a real thing."
But pharmacists and patients have developed workarounds. You can open the capsule, count the beads, and remove a few at a time for a gentler taper. Or you can dissolve the beads in water and drink a measured portion, reducing your dose by tiny increments.
That's what I did. I opened the capsules, dissolved the beads in water, and sipped. A harm reduction approach when the alternative was cold-turkey withdrawal while already malnourished.
I did the same with thiamine and magnesium supplements, dissolved them so my angry stomach could absorb them slowly instead of rejecting them whole.
Why thiamine? Because weeks of vomiting plus weight loss plus new neuropathy is a classic presentation of gastrointestinal beriberi, AKA thiamine deficiency. The European guidelines say you treat first and test later because delays can cause permanent damage. My provider wanted to test first. The guidelines I cited disagreed with him.
Within days of getting nutrients in and reducing the medication that was flooding my system with norepinephrine, the vomiting stopped. I started sleeping. I started eating. I started feeling like maybe I wasn't dying.
The Part That Makes Me Cry
I'm 29 years old. I've declared medical bankruptcy twice. Not because I have some exotic disease requiring experimental treatment but because I kept getting dismissed until manageable conditions became crises.
The average time to diagnosis for hEDS is 10-12 years and 15 different clinicians. I've seen more than that. 94% of hEDS patients receive at least one psychiatric misdiagnosis before getting the right answer. 88% are told they're making it up. 69% of POTS patients are initially labeled with anxiety.
I am not a statistic. I am a person who spent a decade and a half being told my symptoms were in my head while my body was screaming a consistent, coherent story that no one bothered to listen to.
And the thing that breaks me? I shouldn't have had to figure this out myself. This information exists. It's in peer-reviewed journals. It's in clinical guidelines. It's taught at specialized centers. It's just not making it to the providers who see patients like me.
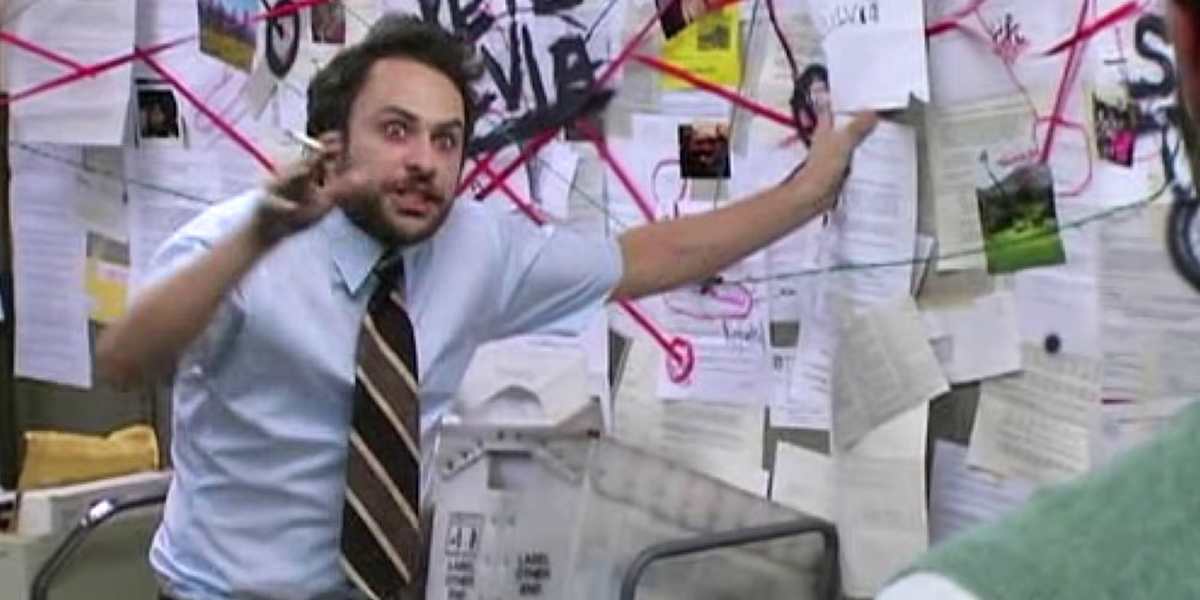
So I became my own specialist. I used AI to help me synthesize research papers, to organize the connections between my conditions, to translate medical jargon into patterns I could see. The same AI tools my provider told me he uses and advocates for. When he uses them, it's innovation. When I use them, it's "inappropriate recommendations."
What I Want You to Know
If you're reading this and you see yourself (the endless appointments, the conflicting diagnoses, the providers who make you feel crazy) I want you to know:
Your research is valid. You're allowed to be educated about your own body. You're allowed to notice patterns your doctors miss. You're allowed to cite medical literature and expect it to be taken seriously.
Your symptoms are connected. If you have a collection of "unexplained" conditions affecting multiple systems, especially if you're a young woman, especially if you're hypermobile, look into hEDS and MCAS. Look into the triad. The answers might be hiding in plain sight.
You are not too much. You are not a difficult patient for advocating for yourself. You are a person who deserves answers, and the system's failure to provide them is not your fault.
Where I Go From Here
I'm not cured. hEDS doesn't work like that... you don't fix your collagen with willpower. But I understand now. I understand why my heart races and my stomach stops and my bladder screams and my nerves burn and my joints slip. I understand that these aren't separate problems but one body doing what it was always going to do, given how it was built.
Understanding changes everything. It means I can stop chasing diagnoses and start managing root causes. It means I can find providers who know this triad and stop wasting time with ones who don't. It means I can stop doubting myself every time someone in a white coat looks at me like I'm nutso.
I slept last night. I ate today. I figured out what was wrong with me when no one else would.
I'm so fucking proud of myself.
And if you're out there fighting the same fight, I'm proud of you too.
—
For everyone who's ever been told it's all in their head: Keep looking. The answers are out there. Sometimes you just have to find them yourself.